Dural venous sinus stenting
- Home
- Dural Venous Sinus Stenting
What is dural venous sinus stenting?
Dural venous sinus stenting is a minimally invasive endovascular procedure used to treat conditions caused by narrowing (stenosis) or blockage in the brain’s dural venous sinuses. These large veins are responsible for draining blood from the brain, and when they become narrowed, it can lead to increased intracranial pressure, causing severe headaches, vision problems, and neurological symptoms.
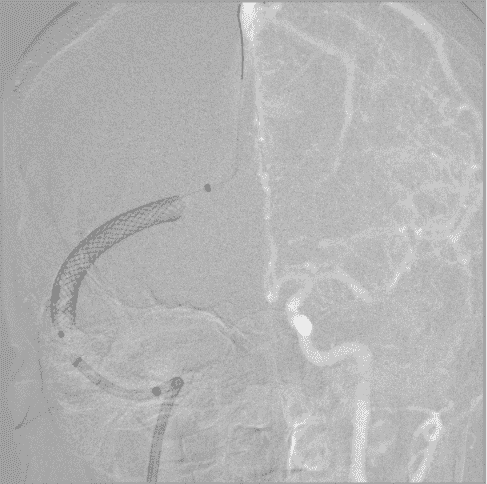
This procedure is commonly performed for patients with Idiopathic Intracranial Hypertension (IIH) associated with significant venous sinus stenosis (a condition also known as pseudotumor cerebri), where elevated pressure inside the skull can lead to debilitating symptoms. During the procedure, a small metal stent is placed within the narrowed venous sinus to restore normal blood flow, reducing pressure and relieving symptoms.
Dural venous stenting is performed using catheter-based techniques, usually via the femoral vein, and guided by advanced imaging like cerebral angiography. It is a highly effective treatment with a good success rate, often improving headaches, vision disturbances, and other pressure-related symptoms significantly.
What Are the Causes of Dural Venous Stenosis?
Dural Venous Stenting is performed to treat dural venous sinus stenosis, which occurs when the large veins responsible for draining blood from the brain become narrowed or blocked. Several factors can contribute to this condition, leading to increased intracranial pressure and the need for stenting:
01
Idiopathic Intracranial Hypertension (IIH)
A condition where cerebrospinal fluid (CSF) pressure increases without a known cause, leading to venous narrowing and impaired drainage.
02
Venous Sinus Thrombosis (VST)
Blood clots in the dural venous sinuses can lead to scarring and narrowing, restricting normal blood flow.
03
Congenital Narrowing or Structural Abnormalities
Some individuals are born with naturally narrowed venous sinuses, predisposing them to increased intracranial pressure.
04
Chronic Inflammation or Infections
Conditions like meningitis or other inflammatory disorders can cause thickening and narrowing of the venous sinuses.
05
Secondary Causes
Head trauma, tumors, or previous surgical procedures can contribute to stenosis by compressing or damaging the dural venous sinuses.
Signs and Symptoms of Dural Venous Sinus Stenosis
Dural venous stenosis occurs when the large veins responsible for draining blood from the brain become narrowed or blocked, leading to increased intracranial pressure. The symptoms can vary based on severity but often include the following:
1. Persistent Headaches – One of the most common symptoms, often described as a pressure-like headache that worsens when lying down or bending over.
2. Pulsatile Tinnitus (Whooshing Sound in the Ears) – A rhythmic whooshing or throbbing sound in the ears, matching the heartbeat, due to turbulent blood flow.
3. Vision Problems – Blurred vision, double vision, or episodes of temporary vision loss due to increased pressure on the optic nerves (papilledema).
4. Dizziness and Balance Issues – Patients may experience lightheadedness, difficulty walking, or a sensation of unsteadiness.
5. Cognitive Difficulties – In some cases, memory problems, difficulty concentrating, or brain fog may occur due to impaired blood drainage.
6. Facial Pressure or Pain – Some individuals report a feeling of fullness or discomfort around the forehead and temples.
7. Seizures or Neurological Deficits (Rare Cases) – If blood flow is significantly impaired, it may trigger seizures or stroke-like symptoms, such as weakness or numbness on one side of the body.
Treatment Options for Dural Venous Stenosis
The treatment for dural venous stenosis focuses on relieving symptoms, reducing intracranial pressure, and restoring normal blood flow. Depending on the severity of the condition, doctors may recommend the following approaches:
01
Medications (Conservative Management)
Diuretics (Acetazolamide, Furosemide) – These help reduce cerebrospinal fluid (CSF) buildup and lower intracranial pressure.
Blood Thinners (Anticoagulants) – If the stenosis is associated with blood clot formation, anticoagulants like warfarin or heparin may be used.
02
Endovascular Dural Venous Stenting (Minimally Invasive Procedure)
A catheter is inserted into the narrowed vein, and a stent (small mesh tube) is placed to widen the vessel and improve blood drainage.
This procedure is commonly performed for patients with intracranial hypertension, pulsatile tinnitus, or vision-threatening papilledema.
It is a minimally invasive procedure with a high success rate and rapid recovery time.
03
Surgical Interventions (For Severe Cases)
Shunt Surgery – A cerebrospinal fluid (CSF) shunt may be implanted to divert excess fluid and relieve pressure.
Venous Bypass Surgery – In rare cases, an alternative blood flow route may be created if stenting is not an option.
04
Lifestyle and Supportive Measures
Weight Loss – In cases related to idiopathic intracranial hypertension, weight loss is very useful in reducing symptoms.
Regular Monitoring – Patients may need follow-up imaging (MRV, CT Venography) to monitor blood flow and assess the effectiveness of treatment.
FAQs
01. Will dural venous stenting cure my symptoms permanently?
For many patients, dural venous stenting provides a durable and long lasting cure. In most cases of IIH, stenting of one venous sinus is good enough, however in rare cases, bilateral stenting of the transverse sinuses may be required. Further, regular follow-ups are necessary to monitor the stent and ensure continued improvement.
02. Are there any lifestyle changes needed after the procedure?
Patients may be advised to maintain a healthy lifestyle, stay hydrated, and, in some cases, take blood thinners to prevent clot formation in the stent.
03. What are the risks or complications of dural venous stenting?
Potential complications include stent migration, blood clot formation, minor bleeding at the catheter insertion site, and, in rare cases, vein re-narrowing. However, these risks are uncommon with proper medical care.
04.Who needs dural venous stenting?
Patients with conditions like idiopathic intracranial hypertension (IIH), venous sinus stenosis, or chronic headaches due to increased intracranial pressure may benefit from dural venous stenting.
05.Do I need to stay in the hospital after the procedure?
Most patients are monitored for a few hours and discharged the same day, though some may need an overnight hospital stay for observation.
Choosing the Right Treatment for Dural Venous Stenting
Confirming the Diagnosis – Imaging tests like MRV (Magnetic Resonance Venography) or cerebral angiography help identify venous sinus narrowing or blockage.
Evaluating Symptoms – Patients with intracranial hypertension, severe headaches, pulsatile tinnitus (whooshing sound in ears), or vision problems may need stenting.
Medical Management First – Initial treatment often includes medications like blood thinners and diuretics to reduce pressure before considering stenting.
Severity of Venous Narrowing – If venous sinus stenosis is causing significant pressure buildup, stenting may be the best option to restore normal blood flow.
Risks vs. Benefits – Weighing the advantages of relieving pressure and improving symptoms against potential risks like bleeding, infection, or stent migration.
Quick Links
Address
Fortis Hospital – Mulund
Goregaon Link Rd, Nahur West, Industrial Area, Bhandup West, Mumbai, Maharashtra 400078

