Head & Neck Vascular Malformations
- Home
- Head & Neck Vascular Malformations
What are Head & Neck Vascular Malformations
Head and neck vascular malformations are developmental anomalies in the formation of blood vessels or lymphatic vessels in the head and neck region. These malformations occur due to improper development of the vascular system during fetal growth. Some of these may be present at birth, whilst others may become noticeable later in life. Unlike tumors, vascular malformations do not grow uncontrollably but can expand over time, causing functional and aesthetic concerns.
These malformations are classified based on the type of affected vessels, including arteriovenous malformations (AVMs), venous malformations, lymphatic malformations, and capillary malformations. The severity of symptoms depends on the size, location, and type of malformation, with some causing swelling, pain, breathing difficulties, or disfigurement.
Diagnosis typically involves imaging techniques like MRI, CT scans, and Doppler ultrasound to assess the extent and nature of the malformation. Treatment options range from sclerotherapy, embolization, laser therapy, and surgery, depending on the type and severity of the vascular anomaly. Early detection and appropriate medical intervention can help manage complications and improve the patient’s quality of life.
What are the causes ofHead & Neck Vascular Malformations?
Head and neck vascular malformations are congenital abnormalities caused by improper blood vessel or lymphatic vessel development during fetal growth. While the exact cause is not always known, several factors contribute to their formation:
01
Genetic Factors
Certain genetic mutations affect vascular development, leading to abnormal vessel formation. Conditions like Hereditary Hemorrhagic Telangiectasia (HHT), Klippel-Trénaunay Syndrome, or PHACES Syndrome are associated with vascular malformations.
02
Errors in Embryonic Development
During fetal development, the vascular system forms through a complex process of vessel growth and remodeling. Disruptions in this process, such as incomplete vessel regression or excessive vessel proliferation, can lead to malformations in the head and neck region.
03
Hormonal and Environmental Factors
Some malformations, like lymphatic malformations, may be influenced by hormonal changes during puberty or pregnancy. Environmental factors, infections, or exposure to certain medications during pregnancy might also contribute to vascular abnormalities.
04
Abnormal Blood Flow Regulation
In some cases, an imbalance in angiogenesis (new blood vessel formation) and vasculogenesis (blood vessel remodeling) results in vascular malformations. This can cause excessive or underdeveloped blood vessel growth, leading to abnormal connections such as arteriovenous malformations (AVMs).
Although these malformations are present at birth, they may not become visible until later in life, especially during periods of rapid growth or hormonal changes. Early diagnosis and medical intervention can help manage symptoms and prevent complications.
Signs and Symptoms of Head & Neck Vascular Malformations
The symptoms of head and neck vascular malformations vary depending on the type, size, and location of the abnormal blood or lymphatic vessels. While some malformations are noticeable at birth, others may become evident later in life due to growth, trauma, or hormonal changes. Below are the common signs and symptoms:
Visible Swelling or Mass
A soft, compressible, and often painless lump that may grow over time. The swelling may become larger with physical activity, crying, or straining, as increased blood flow fills the malformed vessels.
Skin Changes –
Reddish, bluish, or purplish discoloration of the skin overlying the malformation (especially in venous and arteriovenous malformations). Some malformations may have a warm or pulsating feel due to abnormal blood flow.
Pain or Discomfort–
- Chronic pain or tenderness in the affected area, particularly in venous malformations that develop blood clots (phleboliths).
- Increased discomfort during periods of growth, infection, or trauma.
Functional Impairment–
Difficulty breathing, swallowing, or speaking if the malformation affects the airway, tongue, or throat. Facial asymmetry or deformity due to the progressive growth of the lesion.
Bleeding or Ulceration–
- Arteriovenous malformations (AVMs) and capillary malformations can cause spontaneous bleeding or skin ulceration, especially when exposed to trauma.
Treatment Options for Head & Neck Vascular Malformations
The treatment of head and neck vascular malformations depends on the type, size, location, symptoms, and risk of complications. Some malformations may require monitoring, while others need medical, interventional, or surgical treatment. Here are the primary treatment options:
01
Observation & Conservative Management
- Small, asymptomatic malformations may not need immediate treatment but require regular monitoring for any changes.
- Pain management with anti-inflammatory medications (NSAIDs) or compression therapy can help relieve symptoms.
02
Sclerotherapy (Injection Therapy)
- A minimally invasive procedure where a sclerosing agent (such as ethanol, bleomycin, or doxycycline) is injected into the malformation.
- Effective for venous and lymphatic malformations, causing the vessels to shrink and reduce swelling.
03
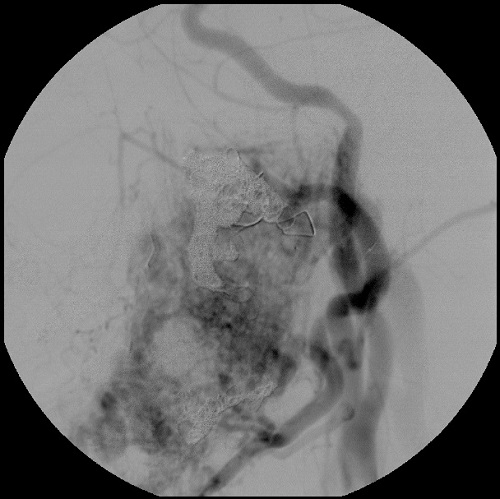
Endovascular Embolization
- Used for arteriovenous malformations (AVMs) to block abnormal blood flow.
- A catheter is inserted through the arteries, and an embolizing agent (glue, coils, or Onyx liquid embolic) is used to close the malformation.
04
Laser Therapy
- Effective for superficial capillary malformations (port-wine stains) and certain venous malformations.
- Laser energy helps reduce discoloration and shrink small abnormal vessels.
05
Medications & Targeted Therapies
- Sirolimus (Rapamycin) is an emerging treatment for complex vascular malformations, particularly lymphatic and venous types.
- Beta-blockers (e.g., propranolol) may be used in certain cases to reduce lesion size and symptoms.
FAQs
01. Do vascular malformations affect speech or breathing?
If they occur near the throat, airway, or vocal cords, vascular malformations may lead to difficulty speaking, swallowing, or breathing, especially if they grow larger.
02. Can vascular malformations bleed?
Yes, some malformations, particularly arteriovenous malformations (AVMs) or large venous malformations (VMs), may rupture and cause bleeding, which can be serious.
03. What lifestyle changes can help manage vascular malformations?
- Avoid trauma to the affected area.
- Monitor growth with regular doctor visits.
- Manage pain with prescribed medications if necessary.
- Consider compression garments (for venous malformations) to improve blood flow.
04. Are vascular malformations hereditary?
Most cases occur sporadically, but some genetic mutations (e.g., in RASA1, PTEN, or TEK genes) can increase the risk, particularly in syndromic conditions like Hereditary Hemorrhagic Telangiectasia (HHT).
Choosing the Right Treatment
The ideal treatment is determined based on:
1) Type & Severity – Venous and lymphatic malformations respond well to sclerotherapy, while AVMs often require embolization and surgery.
2) Location – Malformations near vital structures (e.g., airway, nerves) require careful planning to avoid complications.
3) Symptoms & Risks – If a malformation causes pain, functional impairment, or risk of rupture/bleeding, active treatment is necessary.
Quick Links
Address
Fortis Hospital – Mulund
Goregaon Link Rd, Nahur West, Industrial Area, Bhandup West, Mumbai, Maharashtra 400078

