Spinal cord AVMs
- Home
- Spinal cord AVMs
What are Spinal cord AVMs
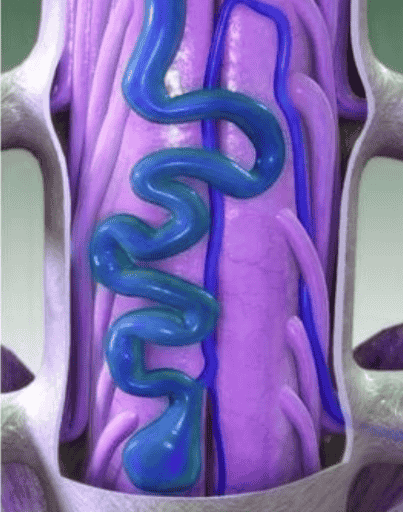
Spinal Cord Arteriovenous Malformations (AVMs) are rare, abnormal tangles of arteries and veins within or near the spinal cord. These malformations disrupt normal blood flow, leading to potential neurological issues due to inadequate oxygen supply and increased pressure on spinal tissues. If left untreated, spinal AVMs can cause progressive weakness, paralysis, or even life-threatening hemorrhages.
The exact cause of spinal AVMs remains unclear, but they are believed to be congenital or develop due to genetic mutations. Symptoms can vary from mild back pain and numbness to more severe complications such as loss of bladder or bowel control. The condition is often diagnosed using MRI or angiography, especially in patients experiencing unexplained neurological symptoms.
Treatment for spinal AVMs depends on their size, location, and severity. Options include endovascular embolization to block abnormal blood flow, surgical resection for complete removal, or radiation therapy to shrink the malformation over time. Consulting an experienced neurovascular specialist, such as Dr. Rajeev Sivasankar, can help determine the best approach for managing spinal cord AVMs effectively.
What are the causes of Spinal cord AVMs ?
The exact cause of Spinal Cord Arteriovenous Malformations (AVMs) is not fully understood, but research suggests that several factors contribute to their development. These abnormal tangles of blood vessels can disrupt normal circulation in the spinal cord, leading to neurological symptoms and potential complications.
01
Congenital Factors
Many spinal AVMs are present at birth due to abnormal blood vessel development during fetal growth. These malformations occur when arteries and veins fail to form correctly, leading to direct connections without capillaries to regulate blood flow.
02
Genetic Mutations
While most spinal AVMs occur sporadically, certain genetic conditions may increase the risk of vascular malformations. Disorders such as Hereditary Hemorrhagic Telangiectasia (HHT) have been linked to the development of AVMs in the brain and spine.
03
Trauma or Injury
In rare cases, spinal AVMs may develop after spinal cord trauma or injury, which could trigger abnormal blood vessel formation as part of the body’s healing response.
04
Vascular Abnormalities & Inflammation
Some researchers believe that abnormal blood vessel growth or chronic inflammation in the spinal cord may contribute to AVM formation over time. Certain inflammatory conditions could weaken blood vessel walls, increasing the risk of malformation.
Signs and Symptoms of Spinal Cord AVMs
The symptoms of Spinal Cord Arteriovenous Malformations (AVMs) vary depending on the size, location, and severity of the malformation. Some individuals may experience mild symptoms, while others may develop serious neurological complications over time. Here are the key signs and symptoms:
1. Progressive Weakness and Numbness
Gradual loss of strength in the legs or arms.
Tingling, numbness, or burning sensations in the limbs.
Muscle weakness that worsens over time, affecting mobility.
2. Pain and Discomfort
Chronic back pain, often in the lower or mid-spine.
Radiating pain down the legs or arms due to nerve compression.
3. Loss of Coordination and Balance
Difficulty walking or maintaining balance.
Unstable movements, increasing the risk of falls.
4. Bowel and Bladder Dysfunction
Loss of bladder control (urinary incontinence) or difficulty urinating.
Bowel dysfunction, including constipation or loss of bowel control.
5. Sudden Paralysis or Sensory Loss
In severe cases, spontaneous paralysis may occur if the AVM causes a spinal hemorrhage (bleeding in the spinal cord).
Loss of sensation in certain areas of the body, especially below the affected region.
Treatment Options for Spinal Cord AVMs
The treatment for Spinal Cord Arteriovenous Malformations (AVMs) depends on factors like size, location, severity of symptoms, and risk of rupture. A combination of medical, surgical, and interventional approaches is used to prevent complications such as paralysis, hemorrhage, or nerve damage.
01
Endovascular Embolization (Minimally Invasive Procedure)
A catheter is inserted through the arteries to reach the AVM.
Special glue, coils, or embolic agents are used to block abnormal blood flow.
Often performed before surgery to reduce bleeding risks.
Best for small-to-moderate AVMs or those in deep spinal regions.
02
Microsurgical Resection (Surgical Removal of AVM)
Open surgery is performed to remove the AVM from the spinal cord.
Used for large AVMs or those causing severe symptoms.
Helps restore normal spinal blood flow and prevent future bleeding.
Best suited for accessible AVMs with a high risk of rupture.
03
Stereotactic Radiosurgery (Non-Invasive Radiation Therapy)
High-dose focused radiation is used to shrink and close the AVM.
Effective for deep-seated or small AVMs where surgery is risky.
Takes months to years for full effects, but reduces hemorrhage risk.
04
Symptomatic & Supportive Treatment
Pain management (medications, physiotherapy).
Physical therapy to maintain mobility and prevent paralysis.
Bowel & bladder management strategies for patients with nerve dysfunction.
FAQs
01. Can Spinal Cord AVMs cause paralysis?
Yes, if left untreated, Spinal Cord AVMs can cause spinal cord damage, leading to progressive weakness, loss of sensation, or even permanent paralysis due to lack of oxygen to the spinal nerves.
02. What are the risks of AVM treatment?
Risks depend on the procedure but may include nerve damage, spinal cord injury, bleeding, infection, or incomplete removal of the AVM. However, timely treatment significantly reduces life-threatening risks.
03. Is Spinal Cord AVM the same as a spinal tumor?
No, a Spinal Cord AVM is a vascular malformation, while a spinal tumor is an abnormal mass of tissue. However, both can cause similar symptoms like weakness, pain, and neurological deficits.
04. What lifestyle changes should AVM patients follow?
Patients should:
- 1) Avoid heavy lifting or high-impact activities that increase pressure on the spine
- 2) Maintain a healthy blood pressure to reduce rupture risks
- 3)Follow regular neurological check-ups to monitor for symptoms
05. Can Spinal Cord AVMs grow over time?
While they may not necessarily “grow,” AVMs can change over time due to increased blood flow, causing worsening symptoms, swelling, or rupture risks.
Choosing the Right Treatment for Spinal Cord AVMs
The choice of treatment depends on:
- Severity of symptoms (pain, weakness, paralysis).
- Risk of rupture (bleeding history, AVM size).
- Patient’s overall health and age.
- Location of AVM (surface vs. deep within the spinal cord).
Quick Links
Address
Fortis Hospital – Mulund
Goregaon Link Rd, Nahur West, Industrial Area, Bhandup West, Mumbai, Maharashtra 400078

