chronic subdural hematoma
- Home
- Chronic Subdural Hematoma
What is chronic subdural hematoma?
Subdural hematoma refers to a condition where blood accumulates between the brain’s dura mater and the underlying tissues. This type of hematoma typically results from head trauma, leading to the rupture of fragile blood vessels. Depending on the severity and duration, it can be classified as acute, subacute, or chronic, each with different levels of risk and treatment approaches.
In most cases, chronic subdural hematomas (cSDH) occur in elderly individuals or those on blood thinners, as minor trauma can cause slow, progressive bleeding. The accumulating blood puts pressure on the brain, which can lead to neurological symptoms like headaches, dizziness, memory loss, or even seizures. Acute subdural hematomas, on the other hand, develop rapidly and may require urgent medical intervention, such as surgery.
A growing treatment option for chronic & recurrent subdural hematomas is Middle Meningeal Artery (MMA) embolization, a minimally invasive procedure where a catheter is used to inject special materials to block the middle meningeal artery, thereby preventing further bleeding and reducing the risk of recurrence. This technique is gaining popularity as an alternative or adjunct to traditional surgical procedures like burr hole drainage. Many centres in Europe, UK & USA are adopting it as the primary modality of treatment in cases where there is little or no neurological deficit associated with cSDHs; or as an adjunct to surgery to prevent re-bleeding.
What are the causes of chronic subdural hematoma
01
Traumatic Head Injury
A direct impact to the head from falls, car accidents, or sports-related injuries can cause bleeding between the dura mater and the brain.
02
Brain Atrophy & Aging
In elderly individuals, the brain shrinks naturally with age, stretching blood vessels and making them more vulnerable to tearing, even with minor head trauma.
03
Anticoagulant Use & Bleeding Disorders
Blood-thinning medications (such as warfarin, aspirin, or heparin) and clotting disorders (like hemophilia or thrombocytopenia) increase the risk of uncontrolled bleeding from the MMA.
04
Chronic Alcoholism
Excessive alcohol consumption weakens blood vessels and affects clotting mechanisms, making even minor head injuries more likely to cause significant bleeding.
05
Repeated Head Trauma
Individuals exposed to frequent concussions or repetitive head injuries, such as boxers, football players, or military personnel, are at higher risk of developing subdural hematomas over time.
06
Brain Surgery & Aneurysm Rupture
Previous neurosurgical procedures or rupture of an aneurysm near the dura can lead to secondary hematoma formation.
Signs and Symptoms of chronic subdural hematomas
The symptoms of Subdural Hematomas depend on the severity of the bleeding, the rate of blood accumulation, and the level of brain compression. While some individuals experience immediate symptoms, others may develop signs gradually over days or weeks.
Early Symptoms –
- Headache – Persistent, worsening headaches, often localized on the side of injury.
- Nausea and Vomiting – Increased pressure in the brain can trigger nausea, sometimes accompanied by vomiting.
- Dizziness and Confusion – Patients may feel disoriented, struggle to concentrate, or experience memory problems.
Progressive Neurological Symptoms –
- Weakness or Numbness – Partial paralysis or loss of sensation, typically on one side of the body.
- Speech Difficulties – Slurred speech, difficulty finding words, or trouble understanding language.
- Visual Disturbances – Blurred or double vision, sensitivity to light, or difficulty focusing.
- Seizures – Uncontrolled jerking movements, convulsions, or sudden loss of consciousness in severe cases.
Severe and Life-Threatening Symptoms –
- Loss of Consciousness – A gradual decline in alertness or sudden collapse, sometimes progressing to coma.
Pupil Abnormalities – One pupil may appear larger than the other, or may not respond to light.
Severe Breathing Problems – Shallow or irregular breathing patterns, indicating high brain pressure.
Delayed Symptoms in Chronic Cases –
- Personality and Mood Changes – Increased irritability, depression, or sudden emotional changes.
- Poor Coordination – Difficulty walking, frequent falls, or loss of balance.
- Cognitive Decline – In older adults, symptoms may mimic dementia, such as memory loss and confusion.
Treatment Options for chronic & recurrent subdural hematomas
The treatment approach for Subdural Hematomas depends on factors such as the size of the hematoma, the severity of symptoms, and the patient’s overall health. Early diagnosis and appropriate intervention can prevent serious complications.
01
Conservative Management (Non-Surgical Treatment)
For small, stable hematomas with mild or no symptoms, doctors may opt for observation and medical management:
- Monitoring: Regular CT scans or MRIs to track changes in the hematoma.
- Medications:
- Blood Pressure Control – To prevent further bleeding.
- Anti-Seizure Drugs – To reduce the risk of seizures.
- Pain Relievers – To manage headaches (avoiding blood-thinning NSAIDs).
- Bed Rest & Head Elevation: Helps reduce intracranial pressure.
02
Minimally Invasive Procedures
If the hematoma is slowly expanding or causing symptoms, minimally invasive options may be considered:
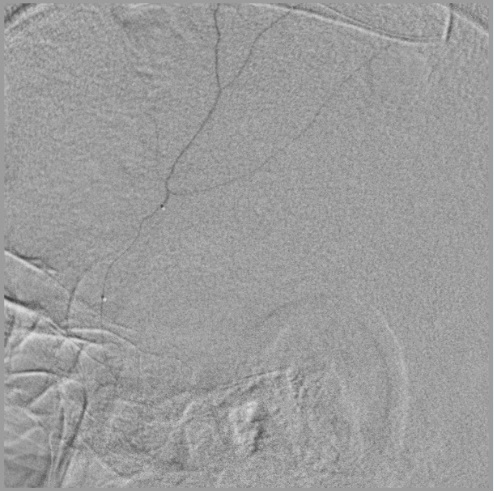
- Middle Meningeal Artery (MMA) Embolization:
- A catheter-based technique where a doctor blocks the MMA using embolic agents (e.g., Onyx, PVA particles).
- Prevents further bleeding and promotes hematoma resolution.
- A catheter-based technique where a doctor blocks the MMA using embolic agents (e.g., Onyx, PVA particles).
- Needle Aspiration (Burr Hole Drainage):
- A small hole is drilled into the skull to drain accumulated blood.
- Often used for chronic subdural hematomas in elderly patients.
- A small hole is drilled into the skull to drain accumulated blood.
03
Surgical Intervention
For large or rapidly expanding hematomas causing significant brain compression, emergency surgery is required:
- Craniotomy:
- A larger skull opening is made to evacuate the hematoma and stop active bleeding.
- Preferred for acute cases with severe neurological impairment.
- Decompressive Craniectomy:
- If brain swelling is severe, a portion of the skull is temporarily removed to relieve pressure.
- Used in life-threatening cases to prevent brain herniation.
04
Rehabilitation & Recovery
After treatment, patients may require:
- Physical & Occupational Therapy – To regain lost motor and cognitive functions.
- Speech Therapy – If language skills are affected.
- Follow-up Imaging – Regular CT/MRI scans to ensure no recurrence.
FAQs
01. How is a Subdural Hematoma diagnosed?
Doctors use CT scans or MRI scans to confirm the presence, size, and location of the hematoma. Additional tests, such as angiography, may be done if MMA embolization is considered.
02. Who is at higher risk of developing a Subdural Hematoma?
- Elderly individuals (brain shrinkage makes veins more vulnerable).
- People on blood thinners.
- Those with a history of head injuries or falls.
- Individuals with bleeding disorders.
03. Can a Subdural Hematoma cause permanent brain damage?
If detected and treated early, most patients recover well. However, severe or recurrent hematomas can lead to lasting cognitive impairment, speech problems, or motor deficits.
04. Can MMA embolization completely cure a subdural hematoma?
MMA embolization can significantly reduce hematoma size and prevent recurrence and aid in complete resolution as seen in recent studies published. However, in some cases, additional procedures like burr hole drainage may be required if the hematoma persists.
05. Are there any dietary or lifestyle restrictions after treatment?
Patients are advised to:
- Avoid blood-thinning medications unless prescribed.
- Maintain good hydration and a healthy diet for brain recovery.
- Limit activities with a high risk of head injury, such as contact sports
Quick Links
Address
Fortis Hospital – Mulund
Goregaon Link Rd, Nahur West, Industrial Area, Bhandup West, Mumbai, Maharashtra 400078

