Intracranial Stenting
- Home
- Intracranial Stenting
What is Intracranial Stenting
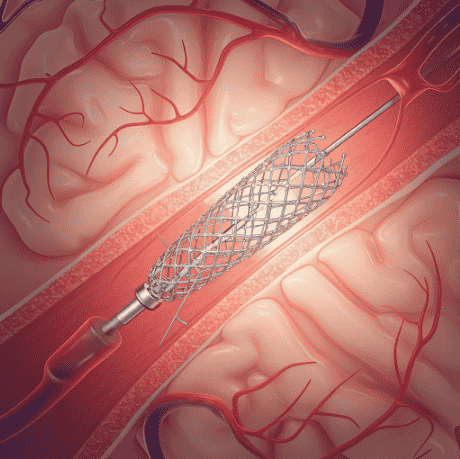
Intracranial stenting is a minimally invasive procedure used to treat narrowed or blocked arteries in the brain, restoring proper blood flow and reducing the risk of stroke. This condition, known as intracranial artery stenosis, occurs due to the buildup of fatty deposits (plaques) inside the blood vessels, leading to reduced oxygen supply to the brain. The procedure involves placing a small mesh-like tube, called a stent, inside the affected artery to keep it open and prevent further blockages.
The stenting procedure is performed using catheter-based techniques, where a thin tube is inserted through the blood vessels (usually via the groin or wrist) and guided to the narrowed artery. Once in place, the stent expands, improving blood circulation. This method is particularly effective for patients who have suffered from transient ischemic attacks (TIAs) or those at high risk of a major stroke due to severe artery narrowing.
Intracranial stenting is often combined with medications like blood thinners to prevent clot formation and improve long-term outcomes. While it offers significant benefits, the procedure carries some risks, including bleeding, vessel damage, or re-narrowing of the artery. Therefore, it is recommended for patients who do not respond well to traditional stroke prevention strategies, such as lifestyle changes and medication therapy.
What Are the Causes of Intracranial Artery Narrowing Requiring Stenting?
Intracranial stenting is performed to treat intracranial artery stenosis, a condition in which the arteries supplying blood to the brain become narrowed or blocked. Several factors contribute to this narrowing, increasing the risk of stroke and other cerebrovascular complications.
01
Atherosclerosis (Plaque Buildup)
The most common cause of intracranial artery narrowing is atherosclerosis, where fatty deposits (plaques) build up inside the arteries, reducing blood flow to the brain.
Risk factors include high cholesterol, hypertension, smoking, diabetes, and obesity.
02
Inflammatory & Autoimmune Disorders
Conditions like vasculitis, lupus, and giant cell arteritis can cause inflammation of blood vessels, leading to narrowing and reduced blood flow.
03
Moyamoya Disease
A rare condition that causes progressive narrowing of brain arteries, leading to an increased risk of stroke.
04
Trauma or Radiation Therapy
Head trauma or prior radiation treatment for brain tumors can cause artery damage and lead to stenosis over time.
Signs and Symptoms of Intracranial Artery Stenosis
Intracranial artery stenosis, the narrowing of blood vessels in the brain, can lead to reduced blood flow and increase the risk of stroke. Symptoms depend on the severity of the blockage and which part of the brain is affected.
1. Stroke Symptoms (When Blood Flow is Severely Blocked)
Paralysis or significant weakness on one side of the body.
Severe, sudden headache (in hemorrhagic cases).
Loss of coordination, leading to falls or difficulty walking.
Difficulty swallowing (dysphagia).
Cognitive problems, including confusion or memory loss.
If the blockage persists or worsens, it can lead to a major ischemic stroke, causing long-term disability.
2. Chronic Symptoms Due to Reduced Blood Flow
Frequent dizziness or vertigo, especially when standing or moving.
Mild but persistent memory or concentration issues due to inadequate oxygen supply to the brain.
Chronic headaches, which may be a sign of compromised circulation.
3. Transient Ischemic Attacks (TIAs) – Warning Signs of Stroke
Temporary weakness or numbness in the face, arms, or legs (often on one side).
Slurred speech or difficulty understanding language (aphasia).
Sudden vision changes, such as blurred or double vision.
Dizziness or loss of balance, making it hard to walk.
TIAs often last a few minutes to hours and resolve without permanent damage but are a serious warning sign of a future stroke.
Treatment Options for Intracranial Stenosis & Stenting
The treatment of intracranial artery stenosis focuses on preventing stroke, improving blood flow, and reducing risk factors. Doctors choose treatment based on the severity of narrowing, presence of symptoms, and overall patient health.
01
Medications (First-Line Treatment for Mild to Moderate Cases)
- Antiplatelet Therapy – Drugs like aspirin, clopidogrel (Plavix), or ticagrelor help prevent clot formation.
- Anticoagulants (Blood Thinners) – Warfarin or newer oral anticoagulants (NOACs) may be used in select cases.
- Statins & Cholesterol-Lowering Drugs – Help reduce plaque buildup and stabilize artery walls.
- Blood Pressure Management – Medications like beta-blockers, ACE inhibitors, or calcium channel blockers to maintain optimal blood flow.
- Diabetes & Lifestyle Management – Controlling blood sugar, quitting smoking, and weight management reduce progression risk.
02
Intracranial Stenting (For Severe Stenosis or Stroke Prevention)
- A minimally invasive endovascular procedure where a stent (small mesh tube) is placed inside the narrowed artery to keep it open.
- Performed along with angioplasty, where a balloon is used to expand the artery before placing the stent.
- Helps restore proper blood flow and reduces the risk of recurrent stroke.
- Recommended for patients who fail medical therapy or have high stroke risk despite medications.
03
Lifestyle & Rehabilitation (Long-Term Stroke Prevention)
- Regular exercise to improve cardiovascular health.
- Healthy diet (low cholesterol, low salt, high-fiber) to reduce plaque buildup.
- Smoking & Alcohol Cessation to lower blood pressure and improve circulation.
- Physical therapy for patients recovering from TIAs or mild strokes.
04
Surgical Options (Rarely Used, High-Risk Cases)
- Bypass Surgery – Creating an alternative blood flow route using a healthy artery from another part of the body.
FAQs
01. How long does the stent last?
Intracranial stents are permanent and designed to keep arteries open. However, lifestyle changes and medications are essential to prevent restenosis and future strokes.
02. Is intracranial stenting better than medication alone?
For mild to moderate cases, medications and lifestyle changes are the first choice. However, patients with severe narrowing and high stroke risk may benefit more from intracranial stenting. The best approach depends on individual risk factors and medical history.
03. Can intracranial stenting be done in an emergency?
Yes. In some cases of acute stroke due to artery blockage, intracranial stenting may be performed as an emergency procedure to restore blood flow quickly.
04. How does intracranial stenting compare to bypass surgery?
Intracranial stenting is less invasive and has a shorter recovery time compared to bypass surgery. However, bypass surgery may be considered for cases where stenting is not effective or possible.
05. Is intracranial stenting a permanent cure?
No. While stenting helps restore blood flow, it does not cure the underlying cause (such as atherosclerosis). Long-term stroke prevention requires lifestyle changes, medication, and regular monitoring.
Choosing the Right Treatment intracranial stenting
Assessing the Severity of Blockage – A thorough evaluation is needed to determine if the artery is significantly narrowed, increasing the risk of stroke.
Medical History and Risk Factors – Factors like high blood pressure, diabetes, smoking, and prior strokes help in deciding if stenting is the best option.
Imaging Tests – Tests like MRI, CT angiography, or cerebral angiography provide a detailed view of the affected artery to confirm the need for a stent.
Symptoms and Stroke Risk – Patients with transient ischemic attacks (TIAs) or minor strokes may benefit from stenting to prevent future strokes.
Alternative Treatments – Doctors consider options like medications (blood thinners, cholesterol-lowering drugs), lifestyle changes, or bypass surgery before recommending stenting.
Quick Links
Address
Fortis Hospital – Mulund
Goregaon Link Rd, Nahur West, Industrial Area, Bhandup West, Mumbai, Maharashtra 400078

