Cerebral venous thrombosis (CVT)
- Home
- Cerebral venous thrombosis (CVT)
What is Cerebral Venous Thrombosis (CVT)
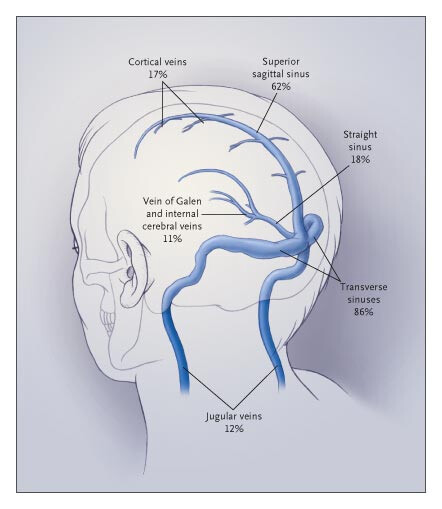
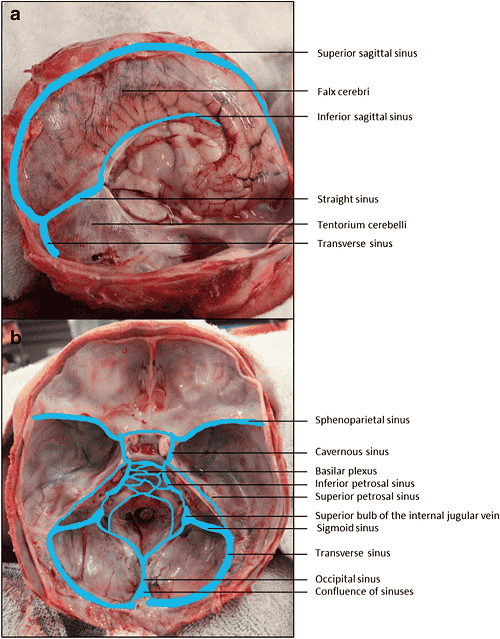
Cerebral Venous Thrombosis (CVT) is a rare but serious condition where a blood clot forms in either the cortical veins or venous sinuses (or both) of the brain, preventing proper drainage of blood. This blockage can lead to increased pressure, brain swelling, or even hemorrhage. Unlike arterial strokes, which occur due to blocked arteries, CVT affects the veins, making its diagnosis and treatment different from other types of strokes.
CVT can develop due to various factors, including blood clotting disorders, infections, head trauma, pregnancy, or certain medications like oral contraceptives. The condition disrupts normal blood circulation in the brain, leading to a buildup of pressure that can cause severe headaches, neurological impairments, and, in some cases, seizures. Early detection and intervention are critical in managing CVT effectively.
Although CVT is life-threatening if untreated, most patients recover well with proper medical care. Treatment typically involves anticoagulant medications to dissolve clots, manage symptoms, and prevent complications. In severe cases, more aggressive treatments such as thrombolysis or surgical procedures may be required. Timely diagnosis through imaging tests like MRI or CT venography significantly improves patient outcomes, ensuring better recovery prospects.
What are the causes of Cerebral Venous Thrombosis (CVT)?
Cerebral Venous Thrombosis (CVT) occurs when a blood clot forms in the brain’s venous system, preventing normal blood drainage and leading to increased pressure or potential hemorrhage. While the exact cause varies among individuals, several key factors contribute to its formation:
01
Genetic Factors
Inherited blood clotting disorders, such as Factor V Leiden mutation or thrombophilia, can increase the risk of CVT.
02
Hypercoagulable Conditions
- Conditions like antiphospholipid syndrome, protein C or S deficiency, and other clotting abnormalities may trigger CVT.
03
Pregnancy & Hormonal Changes
The increased clotting tendency during pregnancy, postpartum recovery, or the use of oral contraceptives and hormone replacement therapy can elevate the risk.
04
Infections & Inflammation
Severe infections like meningitis, sinus infections, or autoimmune diseases such as lupus can lead to inflammation in brain veins, contributing to clot formation.
05
Head Trauma or Surgery
Brain injuries or prior neurosurgical procedures can damage veins, making them prone to clotting.
06
Dehydration & Chronic Illnesses
Conditions like cancer, kidney disease, or inflammatory bowel disease, as well as severe dehydration, can thicken the blood and increase clot risks.
07
Unknown Causes
In some cases, the exact cause of CVT remains unclear, and researchers continue to explore additional genetic and environmental factors.
Signs and Symptoms of Cerebral Venous Thrombosis (CVT)
The symptoms of Cerebral Venous Thrombosis (CVT) can vary depending on the severity of the clot, the location of the blocked vein, and the extent of brain pressure. While some people may experience mild symptoms, others can develop life-threatening complications. Here are the key signs and symptoms of CVT:
Severe, Persistent Headache – Often one of the earliest symptoms, headaches caused by CVT are usually intense, long-lasting, and may worsen over time.
Vision Problems – Blurred vision, double vision, or even temporary vision loss can occur due to increased pressure inside the brain.
Seizures – Uncontrolled movements, muscle twitching, or full-body convulsions may occur in some patients.
Weakness or Numbness – CVT can cause muscle weakness, numbness, or paralysis, typically affecting one side of the body.
Difficulty Speaking or Understanding Speech – Some individuals may struggle with forming words, slurred speech, or difficulty comprehending language, similar to stroke symptoms.
Loss of Consciousness or Confusion – In severe cases, patients may experience confusion, drowsiness, or even go into a coma.
Swelling or Pain Around the Eyes – If the clot affects veins near the eyes, it may lead to facial swelling, redness, or eye pain.
Treatment Options for Cerebral Venous Thrombosis (CVT)
The treatment for Cerebral Venous Thrombosis (CVT) focuses on dissolving the clot, preventing complications, and addressing underlying causes. Early medical intervention is crucial for better recovery. Here are the key treatment options:
01
Anticoagulant Therapy (Blood Thinners)
First-line treatment: Heparin (IV) or low-molecular-weight heparin (LMWH) is used to prevent further clot formation.
Long-term management: After initial treatment, oral anticoagulants like warfarin or direct oral anticoagulants (DOACs) may be prescribed for several months.
02
Thrombolytic Therapy (Clot-Dissolving Drugs)
In severe cases where anticoagulants are ineffective, thrombolytic agents (e.g., tissue plasminogen activator, tPA) may be used to dissolve the clot.
These drugs are typically administered via catheter directly into the affected vein.
03
Mechanical Thrombectomy (Clot Removal Procedure)
If the clot is large and not responding to medication, endovascular procedures (such as thrombectomy or catheter-directed clot removal) may be performed to physically extract the clot.
04
Symptomatic Treatment
Headache relief: Pain management with analgesics (avoiding blood-thinning NSAIDs like aspirin).
Seizure control: Anti-epileptic drugs (AEDs) may be prescribed for patients who develop seizures.
Managing brain swelling: In severe cases, corticosteroids or surgical decompression (craniotomy) may be required to reduce pressure inside the skull.
05
Addressing Underlying Conditions
If an underlying condition (such as infection, cancer, or autoimmune disease) caused CVT, treating that condition is essential to prevent recurrence.
FAQs
01. Is CVT life-threatening?
While CVT can be serious, early diagnosis and treatment significantly improve outcomes. Delayed treatment may lead to complications like stroke or permanent neurological damage.
02. How long does recovery take?
Recovery varies based on the severity of the condition. Many patients recover within a few months with medication and follow-ups, but some may experience lingering symptoms requiring rehabilitation.
03. Can CVT recur?
Yes, recurrence is possible, especially in individuals with clotting disorders or untreated risk factors. Long-term anticoagulation therapy and lifestyle changes help reduce the risk.
04. What are the early warning signs of CVT?
The most common signs include:
Severe headache (often persistent and different from normal headaches)
Vision problems (blurry vision, double vision, or temporary blindness)
Seizures (uncontrolled body movements or convulsions)
Weakness or numbness (especially on one side of the body)
Difficulty speaking or confusion
05. Can CVT cause permanent brain damage?
In some cases, delayed treatment or severe clotting can lead to long-term neurological issues, including cognitive impairment, movement difficulties, or vision problems.
Choosing the Right Treatment for Cerebral Venous Thrombosis (CVT)
Doctors determine the most effective treatment for Cerebral Venous Thrombosis (CVT) based on several key factors:
Severity & Location of the Clot – Small clots may be managed with anticoa
gulant therapy, while larger or more severe cases may require thrombolysis or mechanical thrombectomy to remove the clot.
Risk of Complications – If there are signs of brain swelling, seizures, or hemorrhage, additional treatments like corticosteroids, anti-seizure medications, or even surgical intervention may be necessary.
Patient’s Overall Health – Age, underlying conditions (such as blood disorders, infections, or autoimmune diseases), and the patient’s response to initial treatment help guide further medical decisions.
Early diagnosis and prompt treatment improve recovery outcomes and reduce the risk of long-term complications.
Quick Links
Address
Fortis Hospital – Mulund
Goregaon Link Rd, Nahur West, Industrial Area, Bhandup West, Mumbai, Maharashtra 400078

