Carotid Stenting
- Home
- Carotid Stenting
What is Carotid Stenting ?
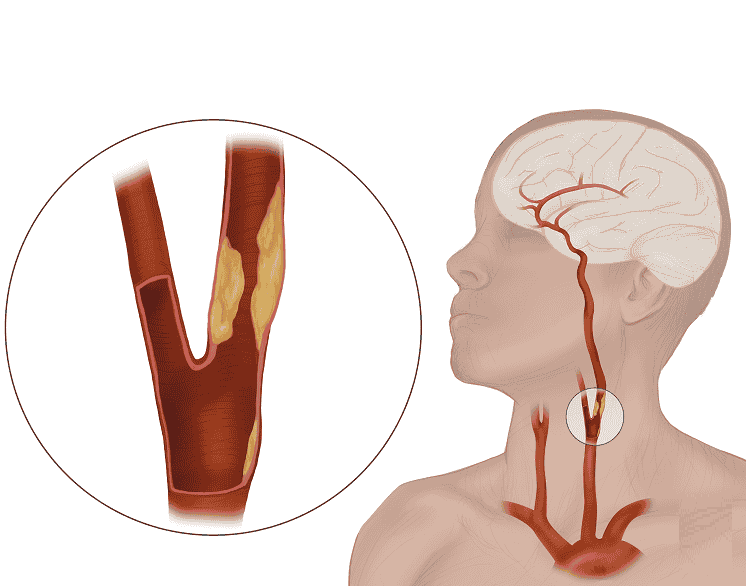
Carotid stenting is a minimally invasive procedure used to treat carotid artery disease, a condition where the carotid arteries (major blood vessels supplying the brain) become narrowed due to plaque buildup (atherosclerosis). This narrowing increases the risk of stroke by reducing blood flow or causing clots to form and travel to the brain. Carotid stenting involves placing a small, mesh-like tube (stent) inside the artery to keep it open, ensuring proper blood circulation and reducing the risk of stroke.
The procedure is typically performed using a catheter inserted through a small incision in the groin or wrist. A balloon is inflated to widen the artery, and then a stent is deployed to maintain the artery’s openness. Carotid stenting is often recommended for patients who are at high risk for traditional carotid surgery (carotid endarterectomy) due to medical conditions like heart disease or previous neck surgeries.
Carotid stenting offers several benefits, including shorter recovery times, reduced surgical risks, and a lower chance of complications compared to open surgery. However, patient selection is crucial, as certain individuals with heavily calcified plaques or high-risk anatomy may not be ideal candidates. Regular follow-ups and lifestyle changes, such as managing blood pressure and cholesterol, are essential for long-term success.
When is Carotid Stenting Required?
Carotid stenting is required when the carotid arteries become narrowed or blocked due to various underlying conditions. The primary causes include:
01
Atherosclerosis (Plaque Buildup)
The most common cause of carotid artery narrowing is atherosclerosis, where fatty deposits, cholesterol, calcium, and other substances accumulate along the artery walls. Over time, this plaque hardens, reducing blood flow and increasing the risk of stroke.
02
Hypertension (High Blood Pressure)
Chronic high blood pressure exerts excessive force on artery walls, leading to damage and making it easier for plaque to accumulate. This weakens the arteries and contributes to their narrowing over time.
03
Smoking and Tobacco Use
Smoking damages blood vessels, promotes inflammation, and accelerates the buildup of plaque in the arteries. It also increases the risk of blood clot formation, further narrowing the arteries.
04
Diabetes and Insulin Resistance
High blood sugar levels contribute to arterial damage and promote atherosclerosis. People with diabetes are at a higher risk of carotid artery disease due to increased plaque formation and poor circulation.
05
High Cholesterol and Poor Diet
Elevated levels of LDL (“bad”) cholesterol and low levels of HDL (“good”) cholesterol contribute to fatty deposits in the arteries. Diets high in saturated fats, trans fats, and processed foods can accelerate plaque buildup.
06
Genetic and Family History
A family history of carotid artery disease, stroke, or other cardiovascular conditions increases the risk of developing arterial blockages that may require stenting.
02
Lack of Physical Activity and Obesity
A sedentary lifestyle contributes to weight gain, high cholesterol, and hypertension—all of which increase the risk of carotid artery disease. Obesity also promotes inflammation and metabolic imbalances that affect vascular health.
05
Prior Stroke or Transient Ischemic Attack (TIA)
Patients who have had a stroke or TIA (“mini-stroke”) are at higher risk of future strokes due to underlying carotid artery disease. In such cases, carotid stenting may be recommended to prevent further blockages.
Signs and Symptoms of Carotid Artery Disease
Carotid artery disease often progresses silently, without noticeable symptoms, until it significantly restricts blood flow or leads to a stroke. Recognizing early warning signs can help prevent serious complications.
Transient Ischemic Attack (TIA)–A Warning Sign –
- Sudden weakness or numbness in the face, arm, or leg, often on one side of the body
- Difficulty speaking or understanding speech (slurred speech)
- Temporary vision loss or blurriness in one or both eyes
- Dizziness, loss of balance, or trouble walking
Stroke Symptoms (If Blockage Becomes Severe) –Sudden and severe headache without a known cause
Loss of coordination, balance, or consciousness
Inability to move or feel one side of the body
Whooshing Sound in the Neck (Bruit) –During a physical exam, a doctor may detect an abnormal “whooshing” sound (bruit) in the neck using a stethoscope. This sound occurs due to turbulent blood flow through a narrowed artery and may indicate an increased risk of stroke.
Silent Progression Without Symptoms –Many people with carotid artery disease do not experience any symptoms until a major event, such as a stroke or TIA, occurs. This makes regular checkups and screenings crucial, especially for individuals with risk factors like high blood pressure, diabetes, smoking, or a family history of cardiovascular disease.
Treatment Options for Carotid Stenosis (Carotid Stenting)
The treatment for carotid artery disease aims to prevent stroke by restoring proper blood flow to the brain. The best approach depends on the severity of the blockage, the patient’s overall health, and the presence of symptoms. Here are the primary treatment options:
01
Medications for Mild to Moderate Blockage
For patients with mild to moderate narrowing of the carotid artery, doctors often recommend medications to manage risk factors and prevent further plaque buildup:
- Antiplatelet Drugs – Aspirin or clopidogrel helps prevent blood clots from forming in narrowed arteries.
- Statins (Cholesterol-Lowering Drugs) – Medications like atorvastatin or rosuvastatin reduce cholesterol and slow plaque buildup.
02
Carotid Stenting (Minimally Invasive Procedure)
Carotid stenting is an endovascular procedure used to open narrowed carotid arteries and prevent strokes. It is recommended for patients who are at high risk for traditional surgery.
- Procedure: A thin, flexible catheter is inserted into the artery through the groin or wrist. A small balloon is inflated to widen the artery, and a metal stent (mesh tube) is placed to keep the artery open.
- Embolic Protection Device (EPD): A small filter is used to catch any loose plaque fragments that could travel to the brain and cause a stroke.
03
Carotid Endarterectomy (Surgical Procedure)
For severe carotid artery blockages (70% or more), a carotid endarterectomy (CEA) may be recommended:
- Procedure: A surgeon makes an incision in the neck, removes the plaque buildup from the carotid artery, and stitches the artery back together.
- Effectiveness: This procedure is highly effective in reducing the risk of stroke for patients with severe carotid stenosis.
04
Lifestyle Changes for Prevention
Regardless of the treatment, long-term prevention strategies are essential:
- Quit Smoking – Smoking increases plaque buildup and worsens carotid artery disease.
- Healthy Diet – A diet rich in fruits, vegetables, and omega-3 fatty acids supports vascular health.
- Regular Exercise – Physical activity helps maintain healthy blood pressure and cholesterol levels.
FAQs
01. How can I prevent further carotid artery disease?
To reduce the risk of future blockages, patients should:
- Quit smoking
- Eat a heart-healthy diet (low in saturated fats and cholesterol)
- Exercise regularly
- Control blood pressure and cholesterol levels
- Manage diabetes if applicable.
02. Can carotid stenting be done on both sides of the neck?
Yes, if both carotid arteries are narrowed, stenting can be done on both sides. However, the procedures are typically performed at different times to reduce the risk of complications.
03. How soon can I return to work after carotid stenting?
Most patients can return to work within a week, depending on their recovery and the nature of their job. Those with physically demanding work may need more time to heal.
04. Can carotid stenting cause dizziness or headaches after the procedure?
Some patients may experience mild dizziness or headaches after the procedure, but these symptoms usually resolve within a few days. Persistent symptoms should be reported to a doctor.
05. Can lifestyle changes alone prevent carotid artery disease?
Lifestyle changes (healthy diet, exercise, quitting smoking) help prevent carotid artery disease but may not reverse severe blockages. In high-risk patients, medical treatment or stenting may still be necessary.
Choosing the Right Treatment for carotid stenting
The decision between medication, carotid stenting, or surgery depends on factors like the degree of blockage, patient health, and stroke risk. Early diagnosis and intervention significantly improve outcomes and reduce the risk of stroke.
Quick Links
Address
Fortis Hospital – Mulund
Goregaon Link Rd, Nahur West, Industrial Area, Bhandup West, Mumbai, Maharashtra 400078

