Cerebral Dural AVFs
- Home
- Cerebral Dural AVFs
What are Cerebral dural AVFs?
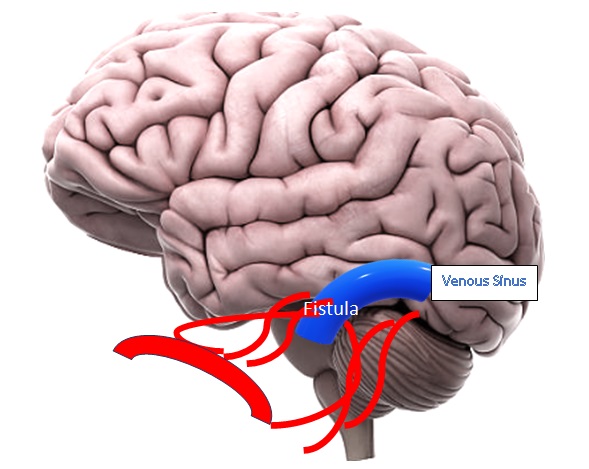
Cerebral Dural Arteriovenous Fistulas (dAVFs) are abnormal connections between arteries and veins within the dura mater, the protective covering of the brain. dAVFs can develop later in life due to various factors, such as trauma, infections, or blood clot-related complications. These abnormal connections lead to increased pressure in the venous system, which can cause neurological symptoms or, in severe cases, life-threatening complications like brain hemorrhages.
The severity of a dAVF depends on its location, size, and the pattern of venous drainage. Some dAVFs have benign courses and cause mild symptoms like headaches or tinnitus (a pulsing sound in the ear), while others can be aggressive, leading to seizures, neurological deficits, or stroke-like symptoms. The key concern with high-risk dAVFs is their ability to drain into deep cerebral veins, which increases the chance of brain swelling or hemorrhage.
The exact cause of dAVFs remains unclear, but they are often associated with conditions that increase venous pressure, such as venous sinus thrombosis (a clot in the brain’s venous system) or previous head injuries. Some theories suggest that abnormal angiogenesis (new blood vessel formation) in response to injury may play a role in their development. In many cases, dAVFs are discovered incidentally during imaging for unrelated neurological conditions, but they require careful evaluation to determine their potential risk.
What are the causes of Cerebral dural AVFs?
The exact cause of Cerebral Dural Arteriovenous Fistulas (dAVFs) is not fully understood, but researchers believe they develop due to abnormalities in the brain’s venous system, often triggered by underlying conditions or external factors. dAVFs are typically acquired later in life rather than present from birth. Below are some key factors that may contribute to their formation:
01
Venous Sinus Thrombosis (Blood Clot in the Brain’s Venous System)
One of the most common causes of dAVFs is venous sinus thrombosis, which occurs when a blood clot blocks one of the brain’s major draining veins.
The blockage increases pressure in the venous system, forcing arteries to form abnormal connections with veins, leading to a dural AVF.
02
Head Trauma & Brain Surgery
- A history of head trauma, skull fractures, or previous brain surgeries can damage the delicate blood vessels in the dura mater.
As the body attempts to heal, new abnormal blood vessel connections may form, resulting in a dAVF.
03
Chronic Inflammation & Infections
Conditions like meningitis, sinus infections, or chronic inflammatory diseases may cause damage to the brain’s blood vessels, increasing the likelihood of abnormal fistula formation.
Inflammation may also contribute to abnormal angiogenesis (new blood vessel growth), leading to the development of a dAVF.
04
Hormonal & Age-Related Changes
Some studies suggest that hormonal fluctuations, particularly in middle-aged and older adults, may influence the formation of dAVFs.
Age-related degeneration of blood vessels and changes in blood flow patterns may also play a role.
05
Unknown & Spontaneous Causes
In many cases, dAVFs develop without an identifiable cause, and researchers continue to study potential genetic, environmental, and vascular risk factors.
Some theories suggest that abnormal pressure regulation in the brain’s venous system may lead to spontaneous fistula formation.
Signs and Symptoms of Cerebral dural AVFs
The symptoms of Cerebral Dural Arteriovenous Fistulas (dAVFs) vary depending on their size, location, and the degree of abnormal blood flow. Some patients may remain asymptomatic for years, while others experience severe neurological complications. Below are the key signs and symptoms:
Pulsatile Tinnitus (Hearing a Rhythmic Sound in the Ear)
One of the most common symptoms of dAVFs is a whooshing or thumping sound in the ear, matching the heartbeat.
This occurs due to the abnormal blood flow near the ear, affecting veins and arteries close to the skull.
Headaches & Increased Intracranial Pressure
Chronic headaches are a frequent symptom, often described as persistent or pressure-like.
In severe cases, dAVFs can cause increased intracranial pressure, leading to nausea, dizziness, or vomiting.
Vision Problems – dAVFs near the eye (cavernous sinus region) can lead to eye bulging (proptosis), redness, or swelling.
Patients may also experience blurred vision, double vision (diplopia), or even vision loss due to venous congestion affecting the optic nerve.
Neurological Deficits & Stroke-like Symptoms
– If a dAVF affects critical areas of the brain, symptoms can resemble a stroke, including:
Muscle weakness or numbness (typically on one side of the body).
Brain Hemorrhage (Severe Cases)– In aggressive dAVFs, the abnormal connection overloads the veins, increasing the risk of brain bleeding (intracranial hemorrhage).
Symptoms of a hemorrhage may include:
Sudden, severe headache (“thunderclap headache”).
Loss of consciousness or fainting.
Treatment Options for Cerebral dural AVFs
The treatment for Cerebral Dural Arteriovenous Fistulas (dAVFs) depends on factors such as the size, location, severity, and risk of rupture. While some low-risk dAVFs can be monitored without immediate intervention, aggressive or symptomatic cases require treatment to prevent serious complications like brain hemorrhage or neurological damage.
01
Endovascular Embolization (Minimally Invasive Procedure)
Primary Treatment – This is the most common and effective method for treating dAVFs.
Procedure – A catheter is inserted through an artery (usually in the groin) and guided to the affected blood vessels. A specialized material (e.g., liquid embolic agents, coils, or glue) is injected to block the abnormal connection.
Benefits – Minimally invasive, quick recovery, and high success rate.
02
Microsurgical Resection (Surgical Removal of dAVF)
When is it Needed? – Recommended for large, high-risk dAVFs that cannot be treated with embolization alone.
Procedure – A craniotomy (small skull opening) is performed, and the surgeon removes or disconnects the abnormal fistula.
Benefits – Effective for dAVFs with high hemorrhage risk.
Risks – More invasive than embolization, requiring longer recovery.
03
Stereotactic Radiosurgery (Targeted Radiation Therapy)
When is it Used? – Ideal for small, deep-seated dAVFs that cannot be reached through surgery or embolization.
Procedure – Precise, high-dose radiation is used to close the abnormal blood vessels over time.
Drawbacks – The closure process is slow, taking months or years, so it is not suitable for urgent cases.
04
Conservative Management (Observation & Monitoring)
When is it Considered? – If the dAVF is asymptomatic, low-risk, and has normal venous drainage, doctors may opt for regular monitoring instead of immediate treatment.
Includes:
Routine MRI/MRA or angiography to track changes.
Lifestyle modifications (avoiding blood thinners or heavy exertion).
Managing symptoms like headaches or tinnitus with medications.
FAQs
01. Can dAVFs recur after treatment?
In some cases, dAVFs can reopen or form new abnormal connections. Regular follow-ups with imaging scans are essential to detect recurrence early.
02. How fast do dAVFs progress?
The progression of dAVFs varies. Some remain stable for years without causing symptoms, while others worsen quickly, leading to brain swelling, vision loss, or hemorrhage if left untreated.
03. Can dAVFs cause tinnitus (ear ringing)?
Yes, many patients with dAVFs experience pulsatile tinnitus, a rhythmic whooshing sound in the ear caused by turbulent blood flow near the auditory system.
04. Is a dAVF the same as an AVM?
No. A Dural AVF forms in the dura mater (outer brain covering) and connects arteries and veins abnormally. A Brain AVM (Arteriovenous Malformation) is a condition with a ‘tangle’ of abnormal blood vessels inside the brain parenchymal tissue.
Choosing the Right Treatment for Cerebral dural AVFs
Doctors decide the best approach based on:
Severity & Risk of Bleeding – High-risk dAVFs need urgent intervention.
Location of dAVF – Some areas are more accessible for embolization or surgery.
Patient’s Overall Health – Age, medical conditions, and response to prior treatments are considered.
Early diagnosis and treatment are crucial to prevent severe complications like brain hemorrhage, vision loss, or stroke. If you or a loved one have symptoms of a dAVF, consult a neurospecialist for the best treatment plan.
Quick Links
Address
Fortis Hospital – Mulund
Goregaon Link Rd, Nahur West, Industrial Area, Bhandup West, Mumbai, Maharashtra 400078

