Cerebral Aneurysm
- Home
- Cerebral Aneurysm
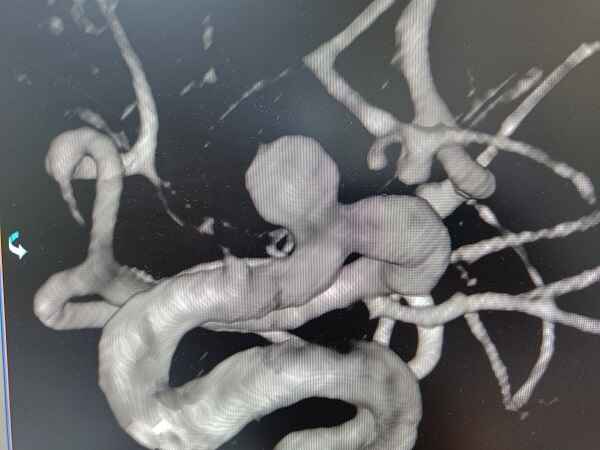
What is a Cerebral Aneurysm?
A cerebral aneurysm is a weakened or ballooned-out section in the wall of an artery supplying blood to the brain. This weakened area can gradually expand due to persistent blood pressure, forming a bulging sac. While some aneurysms remain small and stable without causing symptoms, others grow larger or rupture, leading to a life-threatening medical emergency. A ruptured aneurysm results in bleeding in the brain (subarachnoid hemorrhage), which can cause permanent brain damage, stroke, coma, or even death if not treated promptly.
Most cerebral aneurysms develop over time due to a combination of genetic and lifestyle factors. Conditions such as high blood pressure, atherosclerosis (hardening of the arteries), smoking, and excessive alcohol consumption can weaken blood vessel walls. Some people may also inherit a predisposition to aneurysms due to connective tissue disorders or a family history of the condition. In rare cases, aneurysms can form after head trauma, infections, or complications from certain diseases affecting blood vessels.
Many cerebral aneurysms remain silent, meaning they do not cause noticeable symptoms unless they grow large or begin to leak. When an aneurysm presses on nerves or brain tissue, symptoms may include persistent headaches, vision problems (blurred or double vision), facial pain, difficulty speaking, or weakness in one side of the body. If an aneurysm ruptures, it causes a sudden and severe headache (often described as the “worst headache of one’s life”), nausea, vomiting, stiff neck, confusion, or loss of consciousness. This is a medical emergency requiring immediate intervention.
What are the causes of Cerebral aneurysms?
A cerebral aneurysm occurs when a weakened area in the wall of a brain artery bulges outward, creating a balloon-like sac. Over time, this bulge may grow due to persistent blood pressure, increasing the risk of rupture and leading to a life-threatening subarachnoid hemorrhage (bleeding in the brain). While the exact causes of aneurysm formation vary, several key factors contribute to its development:
01
Genetic Factors
- Individuals with a family history of aneurysms have a higher risk of developing one.
- Inherited connective tissue disorders, such as Ehlers-Danlos syndrome or Marfan syndrome, weaken blood vessels.
- Polycystic kidney disease (PKD) is linked to a greater likelihood of aneurysm formation.
02
Hypertension & Vascular Conditions
- High blood pressure (hypertension) places excess strain on artery walls, making them more prone to bulging.
- Atherosclerosis (hardening of the arteries) due to cholesterol buildup weakens blood vessels.
- Arteriovenous malformations (AVMs)—abnormal connections between arteries and veins—can contribute to aneurysm risk.
03
Smoking & Substance Use
- Cigarette smoking damages blood vessels, increasing the likelihood of aneurysm formation and rupture.
- Excessive alcohol intake raises blood pressure and weakens arteries over time.
- Drug use (especially cocaine and amphetamines) leads to sudden blood pressure spikes, elevating rupture risk.
04
Head Trauma & Brain Injury
- Severe head injuries may weaken blood vessel walls, triggering aneurysm formation.
- Brain surgery or previous vascular procedures can sometimes contribute to aneurysm development.
05
Hormonal & Lifestyle Factors
- Women over 40 are at a higher risk due to hormonal changes that affect blood vessel integrity.
- Obesity, chronic stress, and an unhealthy diet can contribute to poor vascular health, increasing the risk.
- Lack of exercise and sedentary lifestyles may contribute to overall vascular weakening.
06
Infections & Inflammatory Conditions
- Brain infections (meningitis, syphilis, or tuberculosis) can cause vessel inflammation, making them prone to aneurysms.
- Autoimmune diseases (e.g., lupus, vasculitis) may weaken blood vessels, increasing the risk of aneurysm formation.
07
Unknown Causes
In some cases, the exact reason for aneurysm formation remains unclear, and ongoing research aims to identify additional genetic and environmental risk factors.
Signs and Symptoms of Cerebral aneurysms?
The symptoms of a Cerebral Aneurysm depend on its size, location, and whether it has ruptured or is pressing on nearby nerves and brain structures. While many aneurysms remain silent (asymptomatic), others can cause serious neurological complications. The key signs and symptoms are as under:
Unruptured Cerebral Aneurysm – Aneurysms that have not burst may still exert pressure on surrounding tissues, leading to:
Persistent Headaches– Recurring or localized headaches, often described as dull or throbbing.
Vision Problems – Blurred vision, double vision, or loss of peripheral vision due to pressure on the optic nerve.
Pain Around the Eyes – Discomfort behind or above the eyes, sometimes accompanied by eye movement issues.
Facial Numbness or Weakness –If the aneurysm presses on cranial nerves, it may lead to tingling or muscle weakness.
Leaking (Sentinel) Aneurysm – Before a full rupture, an aneurysm may leak a small amount of blood, causing warning symptoms
Drooping Eyelid & Vision Loss–If the aneurysm affects the nerves controlling eye movement.
Treatment Options for Cerebral Aneurysms
The treatment for Cerebral Aneurysms depends on their size, location, rupture status, and overall health of the patient. Early detection and intervention can help prevent life-threatening complications like hemorrhagic stroke. Here are the key treatment options:
01
Monitoring (Watchful Waiting)
For small, unruptured aneurysms that have a low risk of rupture, doctors may recommend regular imaging (MRI, CT angiography) to monitor changes.
Lifestyle modifications, such as controlling high blood pressure, avoiding smoking, and reducing stress, can help minimize the risk of rupture.
02
Surgical Clipping (Open Surgery)
This traditional approach involves placing a small metal clip at the base of the aneurysm to stop blood flow and prevent rupture.
Ideal for aneurysms at risk of rupture or those located in accessible areas of the brain.
03
Endovascular Coiling (Minimally Invasive Procedure)
A catheter is inserted into the artery (usually through the groin) and guided to the aneurysm. Platinum coils are placed inside the aneurysm, causing blood to clot and sealing it off.
This is a less invasive alternative to clipping, with a faster recovery time.
04
Flow Diverters & Stents
Flow-diverting stents are placed in the parent artery to redirect blood flow away from the aneurysm, allowing it to shrink over time.
Suitable for large or wide-necked aneurysms that cannot be treated with coiling or clipping.
05
Emergency Treatment for Ruptured Aneurysms
If an aneurysm ruptures, immediate medical intervention is required to prevent severe brain damage.
Surgical clipping or endovascular coiling is performed urgently to stop the bleeding. Endovascular coiling has been the first line of treatment for these conditions in the past decade and a half due to its minimally invasive nature and lower mortality & morbidity compared to open surgical alternatives.
FAQs
01. Can a cerebral aneurysm go away on its own?
No, aneurysms do not heal or disappear on their own. Small, unruptured aneurysms may remain stable with monitoring, but larger or high-risk aneurysms often require treatment.
02. How long can a person live with a cerebral aneurysm?
Many people live for decades with an unruptured aneurysm if it remains stable. However, if an aneurysm ruptures, immediate medical attention is necessary for survival and recovery.
03. How long does it take to recover from aneurysm surgery?
Recovery varies on various factors such as presence of bleeding, location of the aneurysm, clinical presentation at the time of detection etc:
- Endovascular coiling – 1 to 3 weeks for basic recovery.
- Surgical clipping – 4 to 8 weeks for full healing.
Long-term recovery depends on the patient’s overall health and whether the aneurysm ruptured.
.
04. Can an MRI or CT scan detect a cerebral aneurysm?
Yes, an MRI, MRA (Magnetic Resonance Angiography), CT scan, or cerebral angiography are the most effective imaging tests for detecting aneurysms.
05. Can a cerebral aneurysm cause a stroke?
Yes. If an aneurysm ruptures, it can cause a hemorrhagic stroke, leading to brain damage, neurological impairment, or even death if not treated immediately.
Choosing the Right Treatment for Cerebral Aneurysm
Doctors determine the most effective treatment for cerebral aneurysms based on several key factors:
Size & Location of the Aneurysm – Small, stable aneurysms may only require monitoring, while larger or high-risk aneurysms often need surgical intervention.
Risk of Rupture – If an aneurysm has already ruptured or is showing signs of instability, immediate treatment is necessary.
Patient’s Overall Health – Age, existing medical conditions, and the ability to tolerate surgery or endovascular procedures play a role in treatment selection.
Early diagnosis and timely medical intervention can significantly improve outcomes and prevent serious complications. If you suspect an aneurysm or experience warning symptoms, seek medical attention promptly.
Quick Links
Address
Fortis Hospital – Mulund
Goregaon Link Rd, Nahur West, Industrial Area, Bhandup West, Mumbai, Maharashtra 400078

