Brain Arterio-venous Malformations (AVMs)
- Home
- Brain Arterio-venous Malformations (AVMs)
What are Brain Arterio-venous Malformations (AVMs)
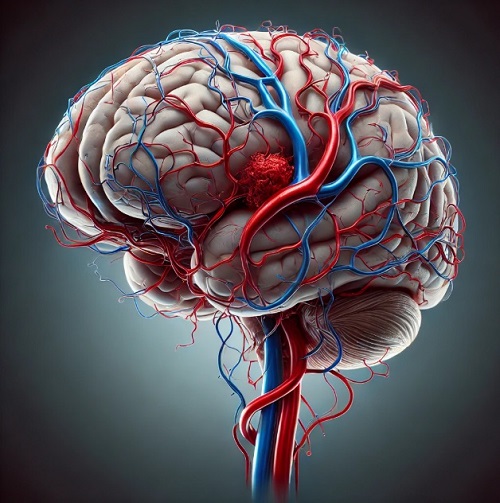
Brain Arteriovenous Malformations (AVMs) are a rare but serious vascular disorder in which a tangled cluster of abnormal blood vessels connects arteries and veins with an intervening abnormal network of vessels called the ‘nidus’. While the exact cause of brain AVMs remains unclear, they are developmental in origin and not congenital as is widely believed. They can occur anywhere in the brain, but their severity and risk largely depend on their size and location.
Diagnosis of a brain AVM typically involves MRI, CT scans, or cerebral angiography, which provide detailed images of the blood vessels. Treatment depends on factors such as the AVM’s location, size, and whether it has caused bleeding. The main treatment options include microsurgical removal, endovascular embolization (blocking abnormal vessels with special materials), and stereotactic radiosurgery (using focused radiation to shrink the AVM). Some small or deep-seated AVMs may be monitored instead of treated if the risks of intervention outweigh the benefits.
Since AVMs are unpredictable, regular monitoring is crucial even if no symptoms are present. While treatment can reduce the risk of bleeding, there is no absolute way to prevent an AVM from forming. Researchers continue to study genetic and environmental factors that may contribute to their development. Individuals diagnosed with a brain AVM should work closely with neurospecialists to determine the best course of action for their condition.
What causes Brain AVMs to form?
The exact cause of Brain Arteriovenous Malformations (AVMs) is not fully understood, but researchers believe they are a developmental condition, which means that due to certain underlying errors in developmental pathways of blood vessels in the brain, some of the vessels do not end up forming mature structures which they were intended to end up as. Hence there is a creation of an abnormal ‘nidus’, an area of fragile, vessels, which links the arteries and vein in a particular area of the brain.. Here are some key factors that may contribute to the formation of brain AVMs:
01
Genetic Factors
While not usually inherited, certain genetic conditions like Hereditary Hemorrhagic Telangiectasia (HHT) can increase the risk of AVMs.
02
Abnormal Blood Vessel Growth
Some AVMs may develop later in life due to unknown factors affecting blood vessel formation.
03
Environmental Triggers (Hypothesis)
Some researchers suggest that brain trauma, radiation exposure, or hormonal changes could contribute, but evidence is limited.
04
Unknown Causes
In many cases, the exact reason for AVM formation remains unclear, and research is ongoing to identify potential risk factors.
Signs and Symptoms of Brain AVMs
Brain AVMs can remain asymptomatic for years, but when symptoms do appear, they vary based on the AVM’s size, location, and whether it has ruptured. Here are the most common signs and symptoms:
1. Neurological Symptoms
Seizures – One of the most common symptoms, ranging from mild to severe convulsions.
Muscle Weakness or Paralysis – Often affects one side of the body (similar to a stroke).
Difficulty Speaking or Understanding Speech – Especially if the AVM is located in language-related brain areas.
Vision Problems – Blurred vision, double vision, or loss of vision in one part of the field.
2. Headache and Bleeding Symptoms
Severe, Sudden Headache – Especially if the AVM ruptures, causing a brain hemorrhage.
Nausea and Vomiting – Can occur due to increased pressure inside the skull.
Loss of Consciousness – May happen if there is significant bleeding in the brain
3. Cognitive and Behavioral Symptoms
Memory Problems – Difficulty retaining or recalling information.
Confusion or Trouble Concentrating – Can be mild or severe, depending on the AVM’s impact on brain function.
Dizziness or Balance Issues – Problems with coordination and movement.
4. Silent AVMs
Some AVMs cause no symptoms and are only discovered during brain imaging for unrelated issues. However, they still pose a risk of rupture.
Treatment Options for Brain AVMs
The treatment for a Brain Arteriovenous Malformation (AVM) depends on factors like its size, location, risk of rupture, and overall health of the patient. Some AVMs may be monitored without immediate intervention, while others require medical or surgical treatment to prevent complications. Below are the primary treatment options:
01
Medications (Symptom Management)
Purpose: Medications do not cure AVMs but help control symptoms.
Common Uses:
Seizure medications – To prevent or manage seizures caused by AVMs.
Pain relievers – To reduce headaches associated with AVMs.
Blood pressure control – To lower the risk of AVM rupture.
02
Stereotactic Radiosurgery (SRS)
Purpose: Uses highly focused radiation to shrink and close off the AVM over time.
Best For:
Small AVMs that are deep within the brain and difficult to access surgically.
Patients at low immediate risk of rupture but needing long-term treatment.
03
Endovascular Embolization
Purpose: Minimally invasive procedure that blocks blood flow to the AVM.
Best For:
AVMs that are too large for radiosurgery.
Small AVMs
Reducing bleeding risk before surgery
04
Microsurgical Removal (Resection Surgery)
Purpose: Complete removal of the AVM through open brain surgery.
Best For:
AVMs that are easily accessible and at high risk of rupture.
When immediate removal is necessary to prevent future bleeding.
FAQs
01. Can a Brain AVM be treated?
Yes, treatment options include:
Medications – To manage symptoms like seizures and headaches.
Stereotactic Radiosurgery (SRS) – Focused radiation to shrink the AVM.
Endovascular Embolization – A minimally invasive procedure to block abnormal blood flow.
Surgical Removal (Resection) – Open brain surgery to remove the AVM completely.
02. What happens if a Brain AVM is left untreated?
If untreated, a Brain AVM can grow, cause neurological symptoms, or rupture, leading to a life-threatening brain hemorrhage (stroke).
03. Can children have Brain AVMs?
Yes, Brain AVMs can be present in children and may be diagnosed in childhood, especially if symptoms like seizures or developmental delays appear. Treatment options for children depend on the AVM’s size and location.
04. How common are Brain AVMs?
Brain AVMs are rare, affecting about 1 in 100,000 people. Many people with an AVM may never experience symptoms and only discover it incidentally through brain imaging for other conditions.
05. Can pregnancy affect a Brain AVM?
Yes, pregnancy can increase blood flow and raise the risk of AVM rupture, especially during labor. Women with an AVM should discuss their condition with a doctor before planning pregnancy.
Choosing the Right Treatment for Brain Arterio-venous Malformations (AVMs)
Doctors decide on the best approach based on:
Size & Location of the AVM – Deep-seated AVMs may be treated with radiosurgery, while surface AVMs are more suitable for surgery.
Risk of Rupture – If an AVM has bled, urgent intervention may be needed.
Overall Health of the Patient – Age and existing medical conditions influence treatment choices.
Quick Links
Address
Fortis Hospital – Mulund
Goregaon Link Rd, Nahur West, Industrial Area, Bhandup West, Mumbai, Maharashtra 400078

