Acute Ischemic Stroke
- Home
- Acute Ischemic Stroke
What is Acute Ischemic Stroke?
Acute Ischemic Stroke (AIS) occurs when a blood clot or other obstruction blocks blood flow to a part of the brain, depriving brain cells of oxygen and nutrients. This blockage, often caused by a thrombus (a clot forming in a blood vessel) or an embolus (a clot traveling from another part of the body), leads to rapid brain damage if not treated immediately. AIS accounts for more than 80% of all strokes, making it the most common type. The severity of damage depends on the duration of the blockage and the affected brain region.
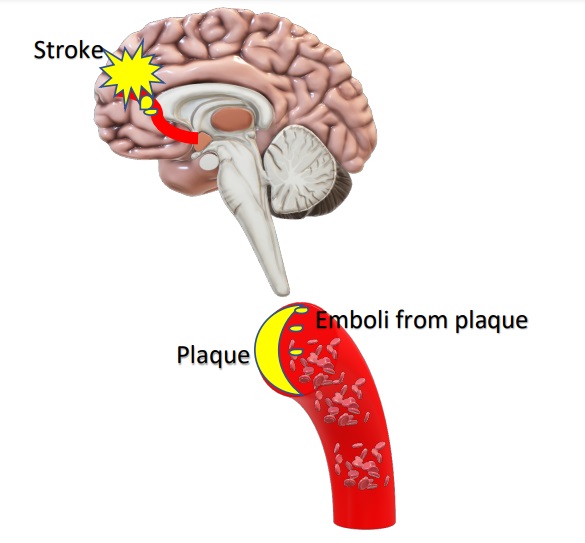
One of the primary causes of embolic stroke to the brain is from underlying atherosclerosis in the vessels of the neck, a condition where fatty deposits (plaques) build up in the arteries, narrowing them and increasing the risk of clot formation. Other risk factors for acute ischemic stroke include high blood pressure, diabetes, smoking, high cholesterol, obesity, and heart diseases such as atrial fibrillation. When a clot obstructs an artery, brain cells begin to die within minutes, leading to potential loss of movement, speech difficulties, cognitive impairments, or paralysis.
Timely treatment is crucial to minimize brain damage. The standard emergency treatment for AIS includes thrombolytic therapy (clot-busting drugs like tPA) and mechanical thrombectomy (clot removal using a catheter-based procedure). Patients often require long-term rehabilitation, including physical therapy, speech therapy, and lifestyle modifications to regain lost functions and prevent future strokes. Early recognition of symptoms—such as sudden numbness, confusion, trouble speaking, or vision problems—and seeking immediate medical attention can significantly improve recovery outcomes.
What are the causes of Acute Ischemic Stroke
Acute Ischemic Stroke (AIS) occurs when blood flow to the brain is obstructed, leading to brain cell damage or death. The most common causes include:
01
Blood Clot Formation (Thrombosis & Embolism)
- Atherosclerosis – The buildup of fatty deposits (plaques) in the arteries can lead to blood clots that block brain blood flow.
- Embolism – A clot or debris (often from the heart or large arteries) travels to the brain, causing a sudden blockage.
- Atrial Fibrillation – An irregular heartbeat can lead to clot formation in the heart, which may break off and travel to the brain.
02
Narrowing of Brain Arteries (Stenosis)
- Carotid Artery Disease – Plaque buildup in the carotid arteries reduces blood supply to the brain, increasing stroke risk.
- Small Vessel Disease – Narrowing of tiny arteries deep in the brain can result in lacunar strokes, often linked to high blood pressure or diabetes.
03
Blood Disorders & Circulation Problems
- Hypercoagulability – Conditions like thrombophilia, sickle cell disease, or high red blood cell count increase clotting risk.
- Low Blood Pressure (Hypoperfusion) – Shock, severe dehydration, or heart failure can cause reduced blood flow, leading to watershed strokes in vulnerable brain areas.
04
Other Contributing Factors
- Smoking, obesity, and high cholesterol accelerate plaque buildup.
- Diabetes damages blood vessels, increasing clot formation.
- Drug Use (e.g., cocaine, methamphetamine) can cause sudden blood vessel constriction or clotting.
Signs and Symptoms of Acute Ischemic Stroke
The symptoms of Acute Ischemic Stroke (AIS) occur suddenly and vary based on the affected brain area. Recognizing these signs early is crucial for immediate medical intervention. The most common symptoms include:
1.Sudden Weakness or Numbness
Weakness or numbness in the face, arm, or leg, often on one side of the body.
Difficulty moving limbs or a sudden loss of coordination and balance.
2. Speech and Communication Problems
Slurred speech or difficulty speaking clearly.
Trouble understanding spoken or written language (aphasia).
Difficulty finding the right words to express thoughts.
3. Vision Changes
Blurred, double, or sudden loss of vision in one or both eyes.
Difficulty focusing or seeing out of part of the visual field (partial blindness).
4. Severe Headache and Dizziness
A sudden, intense headache with no known cause, especially in hemorrhagic conversion.
Feeling lightheaded, dizzy, or experiencing loss of balance.
Trouble walking or frequent falls due to lack of coordination.
5. Confusion and Cognitive Impairment
Sudden difficulty understanding information or following conversations.
Disorientation, memory loss, or trouble concentrating.
Treatment Options for Acute Ischemic Stroke (AIS)
Prompt treatment of Acute Ischemic Stroke (AIS) is crucial to restore blood flow to the brain and minimize long-term damage. The choice of treatment depends on how quickly the stroke is identified and the patient’s overall health.
01
Emergency Medical Treatment
Intravenous Thrombolysis (tPA): The gold standard treatment involves administering tissue plasminogen activator (tPA) within 4.5 hours of symptom onset to dissolve the clot and restore blood flow.
Antiplatelet & Anticoagulant Therapy: Immediate administration of aspirin helps prevent further clot formation. Heparin or Warfarin may be used in selected cases.
02
Mechanical Thrombectomy (Clot Removal)
This is the mainstay of emergency treatment of Acute ischemic strokes in Large vessel occlusions (LVOs). It is a specialized procedure performed within 6-24 hours after symptom onset.
A catheter-based approach is used to physically remove the clot from a blocked artery.
03
Supportive & Rehabilitation Therapy
Blood Pressure Management: Controlling hypertension is essential to prevent further complications.
Physical Therapy: Helps restore movement, coordination, and muscle strength.
Speech & Occupational Therapy: Aids in regaining communication skills and daily function.
Cognitive Therapy: Addresses memory, concentration, and problem-solving deficits.
04
Preventive Strategies to Reduce Recurrence
Lifestyle Changes: Healthy diet, regular exercise, quitting smoking, and limiting alcohol.
Medication Management: Long-term use of statins, blood thinners (Aspirin, Clopidogrel), or anticoagulants for high-risk patients.
Surgical Interventions: Carotid endarterectomy or stenting for patients with carotid artery narrowing to improve blood flow.
FAQs
01. Can ischemic strokes happen more than once?
Yes, without proper treatment and lifestyle changes, recurrent strokes are possible. Long-term medication, regular check-ups, and risk factor management help prevent recurrence.
02. Can young people have an ischemic stroke?
Yes, although stroke is more common in older adults, young adults and even children can suffer from ischemic strokes due to genetic disorders, heart conditions, or clotting abnormalities.
03. Are there any permanent effects after an ischemic stroke?
Some people recover fully, while others may experience long-term effects like paralysis, difficulty speaking, balance issues, and cognitive impairment. Rehabilitation can help improve these conditions.
04. Can an ischemic stroke cause depression or emotional changes?
Yes, post-stroke depression is common due to brain damage, loss of independence, and emotional distress. Psychological support and therapy can help manage these changes.
04. What should stroke survivors do to prevent another stroke?
Follow a doctor’s recommendations, take prescribed medications, control risk factors, and undergo regular medical check-ups to prevent recurrence.
Choosing the Right Treatment for Acute Ischemic Stroke (AIS)
Doctors select the most appropriate treatment based on several key factors:
Time Since Stroke Onset – Intravenous tPA is most effective within 4.5 hours, and works best for small vessel occlusions. FOr larger vessel occlusions mechanical thrombectomy is the mainstay of treatment. Such patients are evaluated in Stroke ready centres and taken to the intervention suite for thrombectomy as early as possible from onset of symptoms. In select patients, with good collaterals, the procedure may be even done within 24 hours from onset.
Severity of Stroke & Blockage Location – Small clots may dissolve with medications, but large vessel occlusions may require thrombectomy to restore blood flow.
Overall Health Condition – Patients with hypertension, diabetes, or heart disease may need customized treatment and long-term blood-thinning therapy to prevent recurrence.
Risk of Bleeding & Other Complications – Thrombolytic drugs carry a risk of bleeding, so doctors assess medical history, brain scans (CT/MRI), and clot location before treatment.
Post-Stroke Recovery & Rehabilitation – After emergency care, physical therapy, speech therapy, and lifestyle modifications play a crucial role in regaining function and reducing future stroke risk.
Early intervention improves survival and recovery! If stroke symptoms appear, seek emergency medical help immediately.
Quick Links
Address
Fortis Hospital – Mulund
Goregaon Link Rd, Nahur West, Industrial Area, Bhandup West, Mumbai, Maharashtra 400078

